How do healthcare professionals make decisions when diagnosing and treating illnesses? Certainly, their continuing medical education helps, and most attend conferences and keep up with research in their field’s peer-reviewed journals.
But professionals also consult guidelines issued by medical societies, such as the International Society for Sexual Medicine (ISSM) or the American Urological Association (AUA). Society panels take a close look at the latest clinical trials and other studies and use that evidence to develop recommendations.
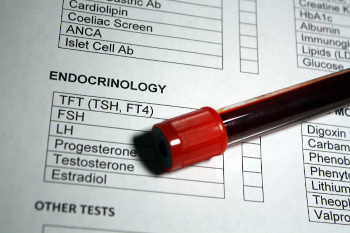
Over the last few years, testosterone replacement therapy has been a hot topic for medical societies. Back in August of last year, we covered new guidelines from the American Urological Society. Today, we’ll discuss a set of guidelines that were updated by the Endocrine Society, a professional group of over 18,000 hormone specialists.
Since testosterone is an important hormone for men, the list of guidelines can be an essential tool for sexual health specialists and primary care physicians who treat men with hypogonadism (low testosterone).
The Endocrine Society guidelines were originally issued in 2010 and updated in 2018.
(Note: For a primer on hypogonadism, please see the links at the bottom of this post.)
Why were the guidelines updated?
Scientists have conducted a great deal of research on testosterone therapy in recent years. The updated guidelines reflect new findings and address concerns.
In addition, more men are seeking help for issues related to testosterone deficiency nowadays, and “low t” gets a lot of media coverage. As a result, men are asking their doctors whether testosterone therapy could help them. It’s critical that prescribers fully understand the benefits and risks.
What do the updated guidelines say?
Highlights of the Endocrine Society’s updated guidelines on hypogonadism include the following points:
Diagnosis
- In general, men shouldn’t be routinely screened for hypogonadism. However, a diagnosis of hypogonadism is recommended if a man has symptoms (such as low libido or fatigue), and a blood test reveals lower-than-normal testosterone levels.
- Based on other hormonal measurements, men can be diagnosed with primary hypogonadism (caused by problems in the testes) or secondary hypogonadism (caused by problems in parts of the brain that trigger testosterone production).
Treatment
- The recommended goals of testosterone therapy are to “induce and maintain” secondary sex characteristics that are driven by testosterone (such as facial hair and muscle mass) and to alleviate symptoms like low sex drive.
- Testosterone therapy is not recommended for men who would like to father a child in the near future. Men with certain health problems (such as prostate cancer, breast cancer, untreated severe obstructive sleep apnea, and recent heart attack or stroke) should not take testosterone.
- Testosterone therapy might not be appropriate for men between the ages of 55 and 69 who are expected to live at least another ten years. Doctors should discuss the benefits and risks with these patients.
- Men over age 65 shouldn’t be prescribed testosterone routinely. Instead, doctors should consider each individual’s situation.
- Men with HIV, low testosterone, and weight loss might undergo testosterone therapy to gain and maintain weight.
- Men with diabetes and low testosterone should not use testosterone as a way to control their blood sugar.
Monitoring
- Once testosterone therapy has begun, men should have regular checkups to make sure it is working well and there are no side effects.
- During the first year of therapy, men with abnormal prostate cancer screening results should see a urologist.
What does this mean for patients?
While these guidelines are intended for healthcare professionals, they can be useful for men, too.
Understanding the guidelines for any treatment you receive helps you weigh the pros and cons of therapy as you make health decisions.
“The [updated Endocrine Society] guideline emphasizes the importance of patient engagement in a shared decision-making process, especially with respect to the choice of treatment regimens and prostate monitoring,” said Dr. Shalender Bhasin, head of the guideline development task force, in an interview with Endocrine News.
Learn more
For more information on hypogonadism and testosterone, please see these links:
Unpacking the Latest Testosterone Therapy Guidelines
What Should Men Know About Topical Testosterone?
Self-Injectable Testosterone Now Available
FDA Approves Testosterone in Pill Form
Resources
Endocrine News
“Q&A: Shalender Bhasin, MD”
(May 2018)
https://endocrinenews.endocrine.org/qa-shalendar-bhasin-md/
The Endocrine Society
“About the Endocrine Society”
https://www.endocrine.org/about-us
“Testosterone Therapy for Hypogonadism Guideline Resources”
The Journal of Clinical Endocrinology and Metabolism
Bhasin, Shalender, et al.
“Testosterone Therapy in Men With Hypogonadism: An Endocrine Society Clinical Practice Guideline”
(Full-text. Published: March 17, 2018)
You may also be interested in...
Other Popular Articles

What Is the Average Penis Size?
If you have ever wondered how your penis compares to others in terms of size, you are not alone. Many men are curious to know how their penises stack up compared to the average. Unfortunately, general curiosity can sometimes give way to full-on obsession and anxiety about penis size. This can be an unhealthy and often unnecessary fixation, especially because most men who think their penises are too small have perfectly normal-sized penises.

What Is Jelqing, and Does It Actually Work?
The term “jelqing” refers to a set of penis stretching exercises that some believe can make the penis bigger. Although the practice has gained attention and popularity in blogs and internet forums in recent years, there is no scientific evidence that it is an effective way to permanently increase the size of one’s penis. In fact, in some cases, jelqing may actually cause damage to the penis, so it is a good idea to get all the facts before setting off to try it.

What Is Sensate Focus and How Does It Work?
Sensate focus is a technique used to improve intimacy and communication between partners around sex, reduce sexual performance anxiety, and shift away from ingrained, goal-oriented sexual patterns that may not be serving a couple.

Can Sex Reduce Menstrual Cramps?
The SMSNA periodically receives and publishes ‘guest editorials.’ The current article was submitted by Mia Barnes, a freelance writer and researcher who specializes in women's health, wellness, and healthy living. She is the Founder and Editor-in-Chief of Body+Mind Magazine.
Having sex while you experience menstrual cramps is healthy and can provide significant benefits. While it might not be the first activity that comes to mind when your PMS or period cramping begins, many people enjoy sex to reduce menstrual cramps, experience increased pleasure and benefit from other advantages. Learn more about having sex while menstrual cramps are happening and how it can help your body.

How Long Does It Take the Average Man to Ejaculate?
On average, it takes a man between 5 to 7 minutes to orgasm and ejaculate during sexual intercourse.

Can Sex Throw off Your Vaginal pH Balance?
The SMSNA periodically receives and publishes ‘guest editorials.’ The current article was submitted by Mia Barnes, a freelance writer and researcher who specializes in women's health, wellness, and healthy living. She is the Founder and Editor-in-Chief of Body+Mind Magazine.
Your vagina is a pretty powerful organ. It is a pathway for menstrual blood and babies. It also is a main player in sexual intercourse. You might hear about your vagina’s pH and worry that yours is at risk. Here’s what to know about vaginal pH, including the impacts sex could have.

