As anyone who has ever tried to navigate health care coverage can attest, it is all too often a frustrating, fruitless endeavor characterized by multiple phone calls, numerous transfers, and invariably long hold times. This cumbersome process creates an obstacle for those seeking medical treatment and may disproportionately affect transgender individuals seeking treatment for gender dysphoria.
A transgender individual is a person whose gender does not align with the sex that they were assigned at birth. This incongruence between gender identity and sex can cause significant psychological distress for a transgender person, which is known as gender dysphoria.
Gender dysphoria can lead to feelings of restlessness, anxiety, and depression. The certainty that one’s true gender is not reflected by one’s body can be an extremely distressing experience that impacts all areas of a person’s life. Transgender individuals may feel disgust towards their genitals and other sex-related physical traits and have a strong desire to be rid of them. This chronic state of stress may lead to thoughts or acts of self-harm, or even suicidality. A 2015 national survey of transgender individuals found that 40% of survey respondents had attempted suicide at least once in their life, with 7% having attempted suicide in the past year.
To compound matters, transgender individuals experience a higher rate of health disparities than the average U.S. citizen. The above-mentioned 2015 survey revealed that 29% of the transgender respondents were living in poverty, and more than half (55%) of those surveyed had been denied coverage for transition-related surgery, while a quarter had been denied coverage for transition-related hormone therapy.
With this information in mind, the authors of a 2020 Journal of Sexual Medicine study set out to determine which U.S. states’ Medicaid programs cover gender-affirming hormone therapy (GAHT) and which cover genital gender-affirming surgery (GAS) for transgender individuals. GAHT and GAS, along with counselling to support transgender people in their transition are the three predominant health services for gender dysphoria at this time.
Results showed that GAHT and GAS are not covered by all state Medicaid programs, and although several states’ Medicaid programs do cover these treatments, the information was often difficult to find, requiring several phone calls and substantial time to track down.
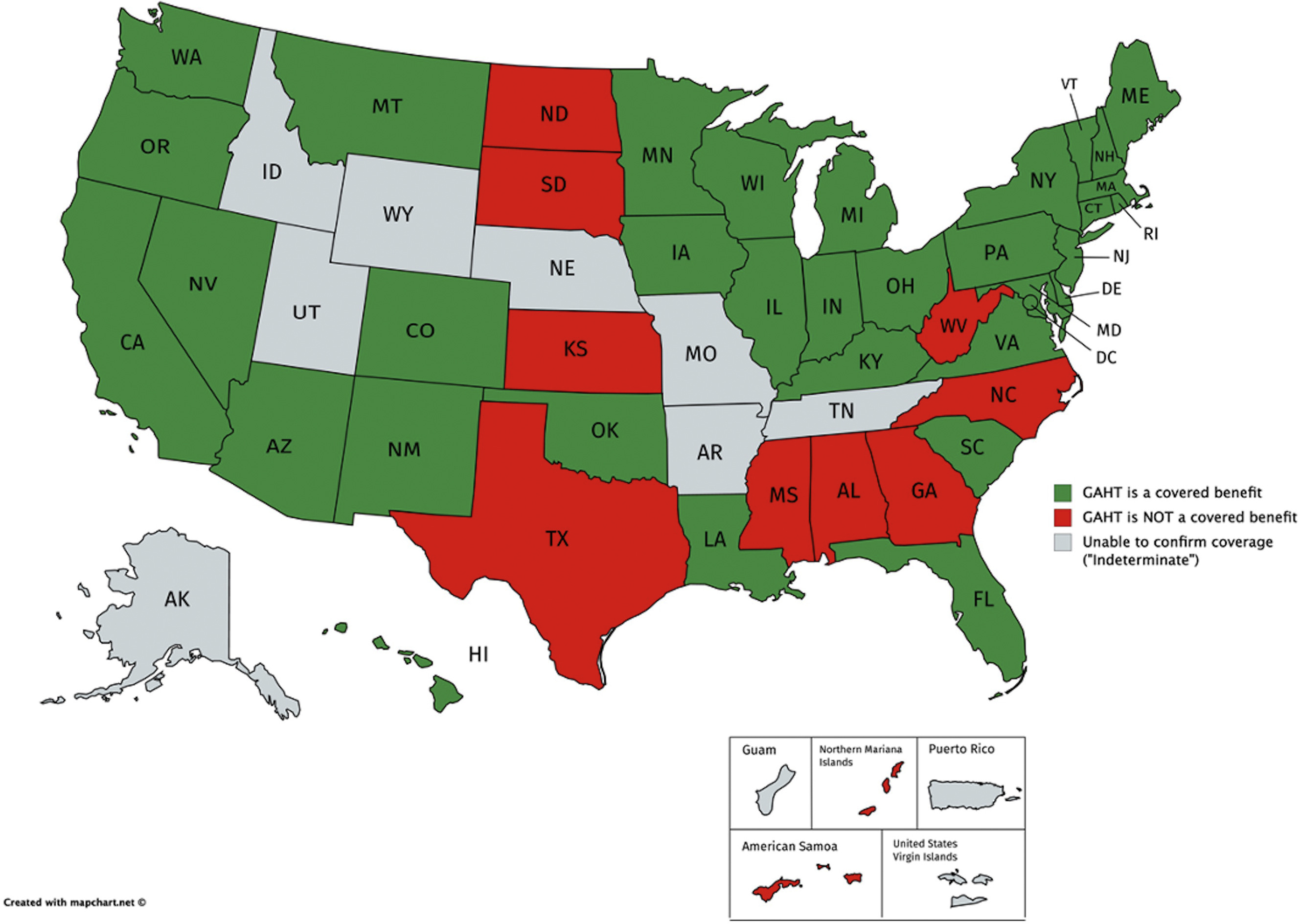
According to this study, GAHT is covered by 34 of 51 state Medicaid programs (including Washington, DC), is not covered by 9 of 51 state programs, and coverage status was deemed “indeterminate” in 8 of 51 states (Figure 1). To find this information, the authors completed an average of 3 phone calls per state (range of 1-10 phone calls) and spent an average of 31.8 minutes on the phone for each unique call (range of 1.5-124.8 minutes).
GAS is even less likely to be covered by Medicaid than GAHT, and it is only covered by 25 of 51 state Medicaid programs. It is not covered by 22 of 51 state programs, and coverage was classified as “indeterminate” in 4 of 51 states (Figure 2). Researchers completed an average of 3.3 phone calls per state to attain this information (range of 1-12 phone calls) and spent an average of 33.2 minutes on the phone during each call (range of 1.5-119.8 minutes).
The authors of this study concluded that several barriers to health care access exist for transgender people and that the process of determining coverage for medical treatments can be very challenging and time-consuming for these patients.
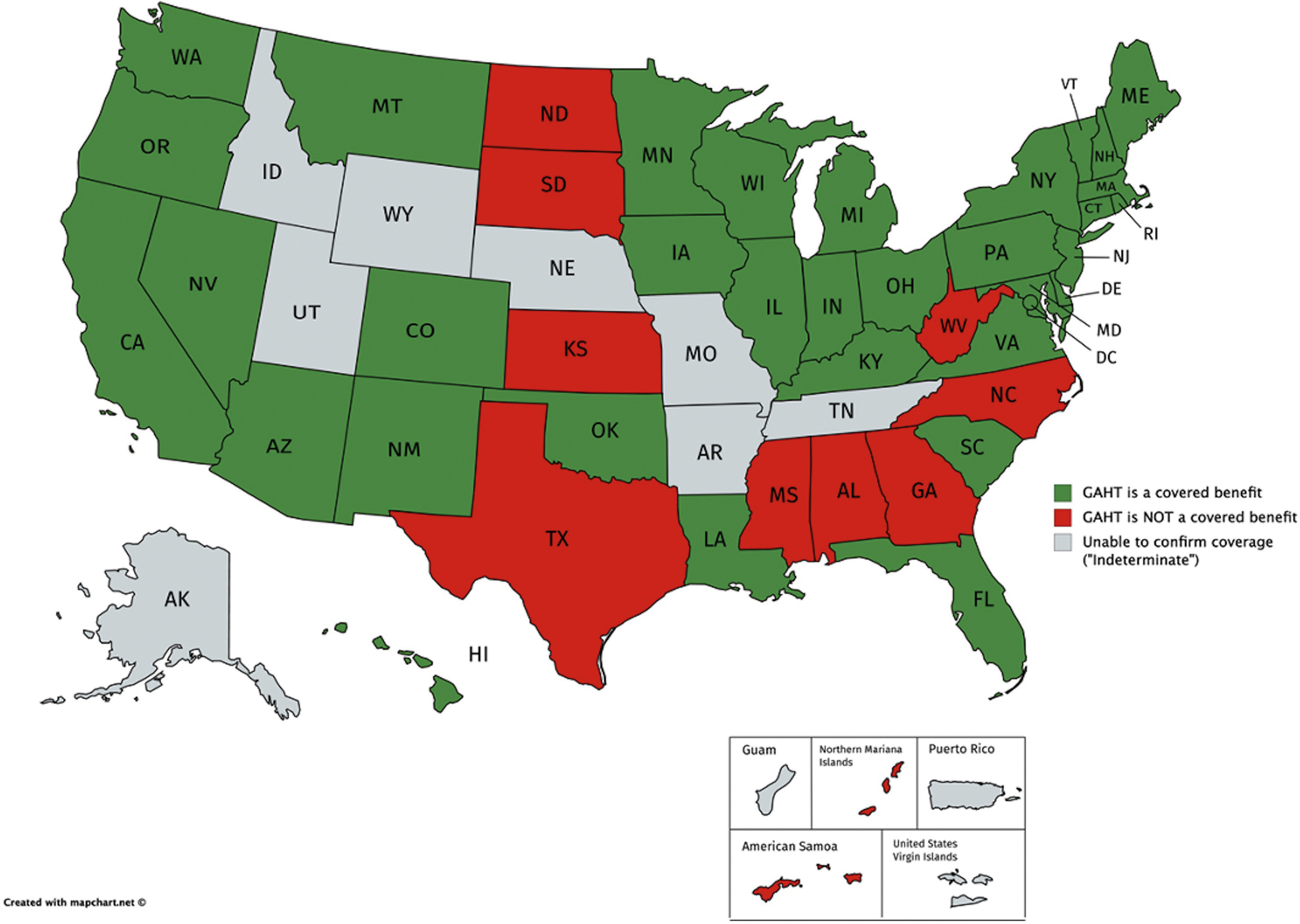
Figure 1. Maps of all 51 U.S. states (includes District of Columbia) and 5 U.S. territories, colored based on whether GAHT is a covered benefit (green), is not a covered benefit (red), or whether coverage remains “indeterminate” (gray). This image was published in The Journal of Sexual Medicine, 18(2), Zaliznyak, M., Jung, E.E., Bresee, C., & Garcia, M.M., Which U.S. States’ Medicaid Programs Provide Coverage for Gender-Affirming Hormone Therapy and Gender-Affirming Genital Surgery for Transgender Patients?: A State-by-State Review, and a Study Detailing the Patient Experience to Confirm Coverage of Services, p. 415, Copyright Elsevier (2021).
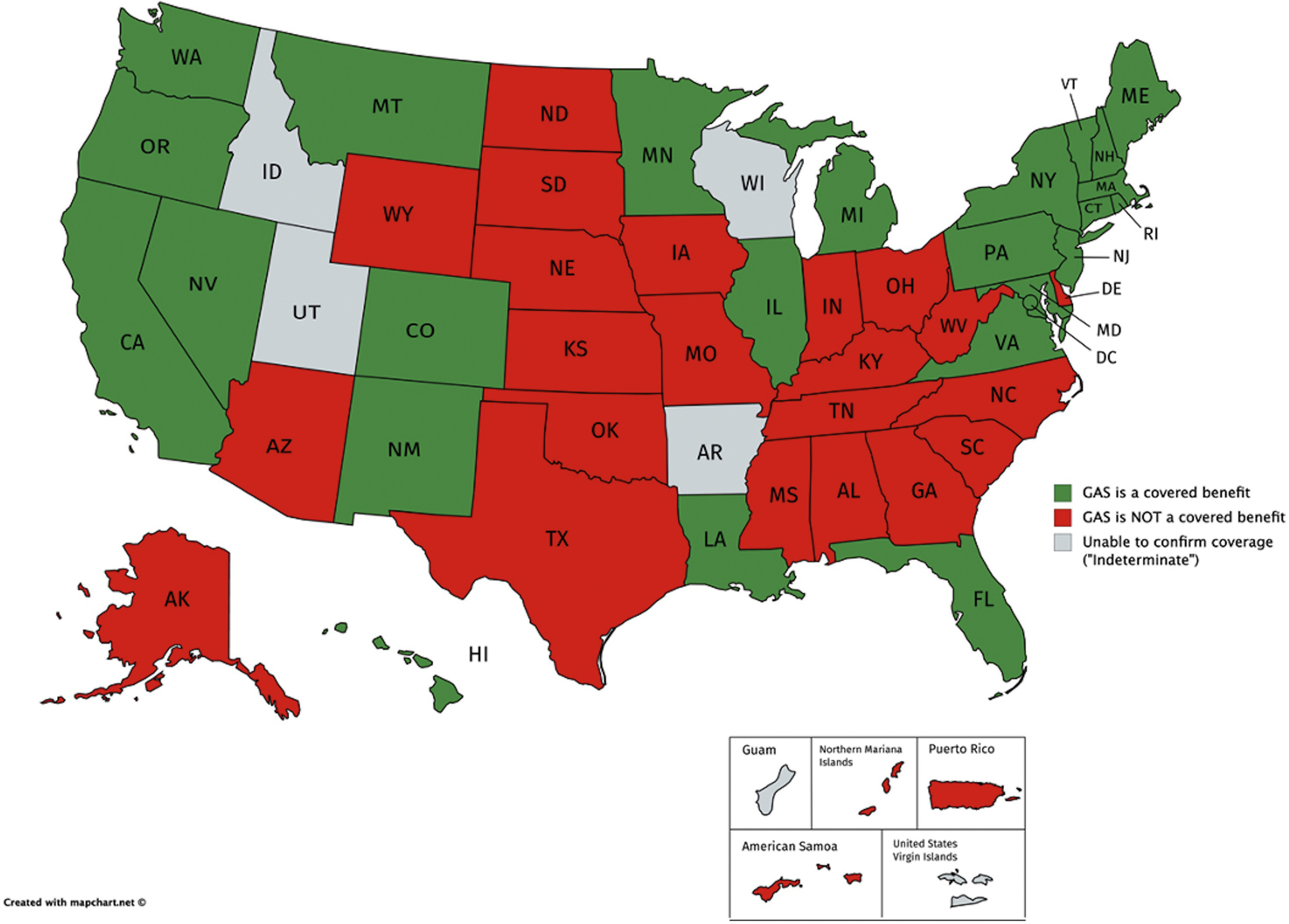
Figure 2. Maps of all 51 U.S. states (includes District of Columbia) and 5 U.S. territories, colored based on whether GAS is a covered benefit (green), is not a covered benefit (red), or whether coverage remains “indeterminate” (gray). This image was published in The Journal of Sexual Medicine, 18(2), Zaliznyak, M., Jung, E.E., Bresee, C., & Garcia, M.M., Which U.S. States’ Medicaid Programs Provide Coverage for Gender-Affirming Hormone Therapy and Gender-Affirming Genital Surgery for Transgender Patients?: A State-by-State Review, and a Study Detailing the Patient Experience to Confirm Coverage of Services, p. 416, Copyright Elsevier (2021).
Resources:
Zaliznyak, M., Jung, E.E., Bresee, C., & Garcia, M.M. (2021). Which U.S. States’ Medicaid Programs Provide Coverage for Gender-Affirming Hormone Therapy and Gender-Affirming Genital Surgery for Transgender Patients?: A State-by-State Review, and a Study Detailing the Patient Experience to Confirm Coverage of Services. The Journal of Sexual Medicine, 18(2), 410-422. https://www.jsm.jsexmed.org/article/S1743-6095(20)31062-6/fulltext
You may also be interested in...
Other Popular Articles

What Is the Average Penis Size?
If you have ever wondered how your penis compares to others in terms of size, you are not alone. Many men are curious to know how their penises stack up compared to the average. Unfortunately, general curiosity can sometimes give way to full-on obsession and anxiety about penis size. This can be an unhealthy and often unnecessary fixation, especially because most men who think their penises are too small have perfectly normal-sized penises.

What Is Jelqing, and Does It Actually Work?
The term “jelqing” refers to a set of penis stretching exercises that some believe can make the penis bigger. Although the practice has gained attention and popularity in blogs and internet forums in recent years, there is no scientific evidence that it is an effective way to permanently increase the size of one’s penis. In fact, in some cases, jelqing may actually cause damage to the penis, so it is a good idea to get all the facts before setting off to try it.

What Is Sensate Focus and How Does It Work?
Sensate focus is a technique used to improve intimacy and communication between partners around sex, reduce sexual performance anxiety, and shift away from ingrained, goal-oriented sexual patterns that may not be serving a couple.

Can Sex Reduce Menstrual Cramps?
The SMSNA periodically receives and publishes ‘guest editorials.’ The current article was submitted by Mia Barnes, a freelance writer and researcher who specializes in women's health, wellness, and healthy living. She is the Founder and Editor-in-Chief of Body+Mind Magazine.
Having sex while you experience menstrual cramps is healthy and can provide significant benefits. While it might not be the first activity that comes to mind when your PMS or period cramping begins, many people enjoy sex to reduce menstrual cramps, experience increased pleasure and benefit from other advantages. Learn more about having sex while menstrual cramps are happening and how it can help your body.

How Long Does It Take the Average Man to Ejaculate?
On average, it takes a man between 5 to 7 minutes to orgasm and ejaculate during sexual intercourse.

Can Sex Throw off Your Vaginal pH Balance?
The SMSNA periodically receives and publishes ‘guest editorials.’ The current article was submitted by Mia Barnes, a freelance writer and researcher who specializes in women's health, wellness, and healthy living. She is the Founder and Editor-in-Chief of Body+Mind Magazine.
Your vagina is a pretty powerful organ. It is a pathway for menstrual blood and babies. It also is a main player in sexual intercourse. You might hear about your vagina’s pH and worry that yours is at risk. Here’s what to know about vaginal pH, including the impacts sex could have.

